The Implant Research Core is committed to providing hands-on training and education on implant retrieval analyses and 3D printing for all levels of students. Every year, the IRC participates in Drexel's STAR (Students Tackling Advanced Research) Scholars Program to provide research project opportunities for undergraduate students. Our project approach is not singularly focused, instead, students are exposed to various research topics by working together and alongside graduate researchers. While the program culminates in a showcase presentation of a particular project, each student comes away with education and hands-on experience on multiple topics relating to orthopaedic devices and 3D printing. Previous projects include:
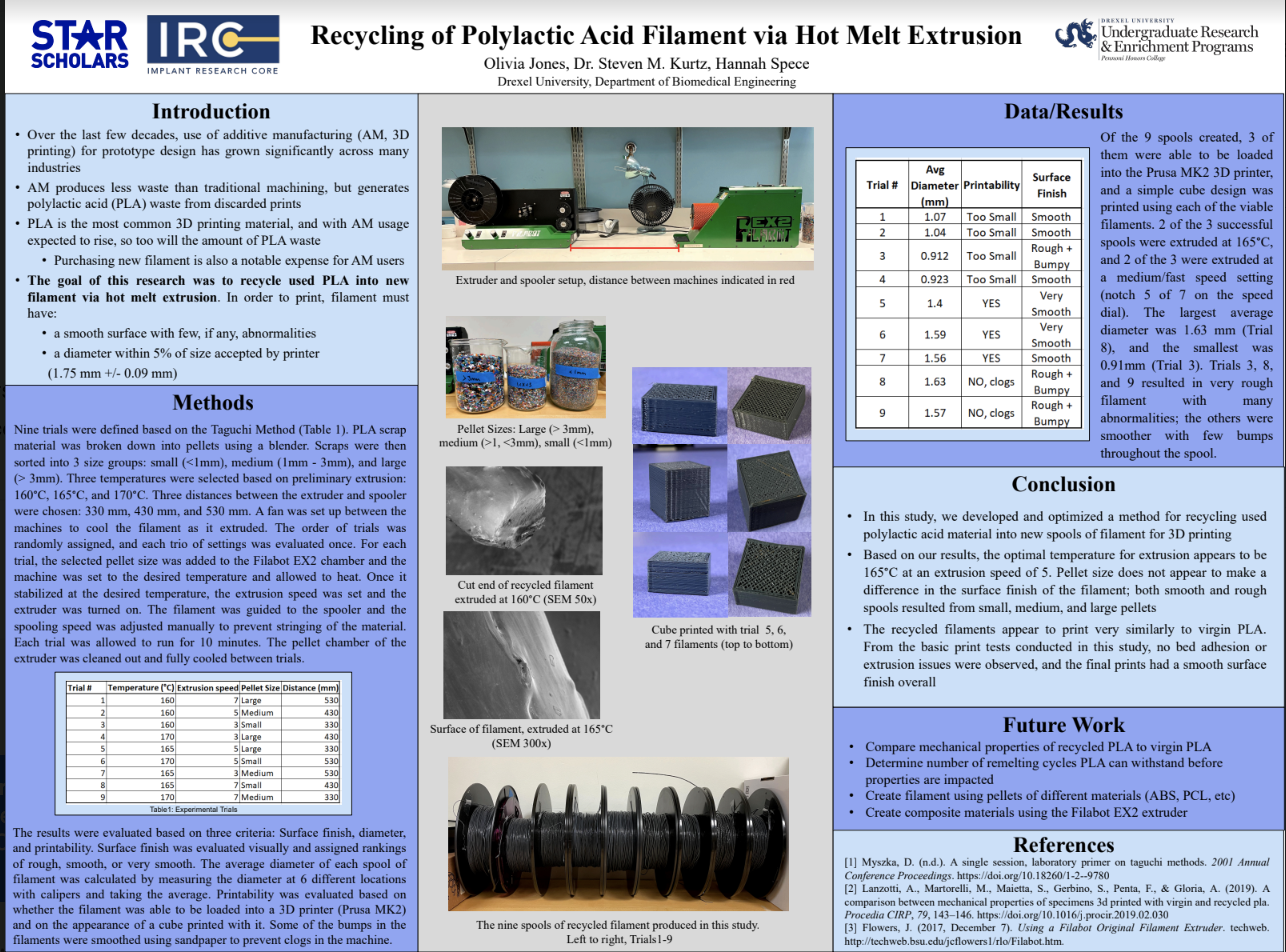
STAR student: Olivia Jones While additive manufacturing (AM, 3D printing) produces less waste than traditional machining, there are concerns regarding the environmental impact of polylactic acide (PLA) waste from discarded prints. PLA is the most common 3D printing material, and with AM usage expected to rise, so too with the amount of PLA waste. Additionally, purchasing new spools of material represents a notable expense for AM users. The goal of this research was to recycle used PLA into new filament via hot melt extrusion. To determine optimal parameters for filament extrusion, 9 trials were defined using the Taguchi method. Variables included temperature, extrusion speed, pellet size, and distance between extruder and spooler. The products of each trial were evaluated for surface finish, diamter, and printability. Results showed that melting the smalles pellets (~1 mm) at 165C gave the smoothest finish, and a diameter similar to commercial filament was achieved with medium-high extrusion speed. Spooling distance did not have a signficant impact on the resulting filament. Future work includes comparing properties of recylced and virgin PLA filament and assessing how many remelting cycles the material can withstand before its properties are impacted.
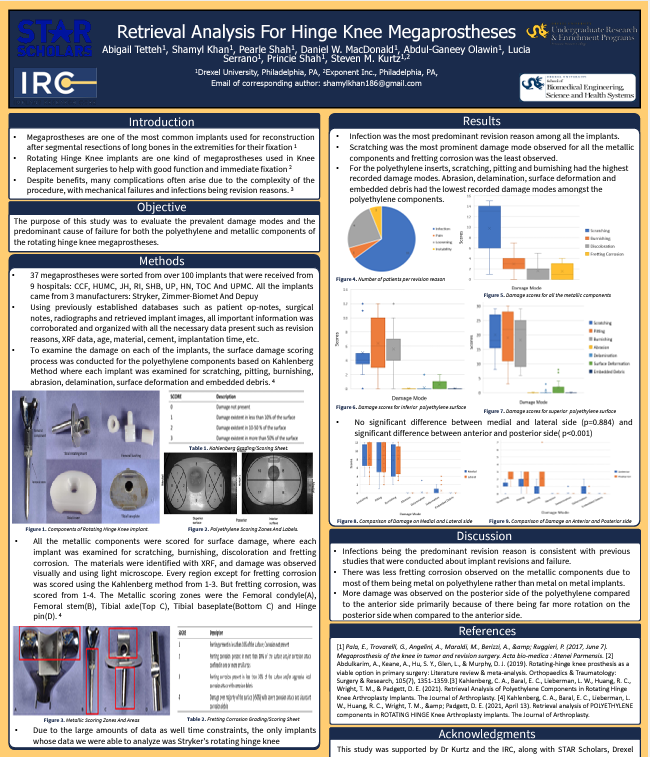
STAR student: Shamyl Khan Distal Femur Fractures (DFFs) account for between 3-6% of all femoral fractures in adults. DFFs can occur in young patients as a result of high impact accidents, however, in elderly patients DFFs often occur due to degenerative diseases such as osteoporosis and arthritis. While a gold-standard consensus has not been made on how to surgically treat DFFs, custom made prosthetics capable of reconstructing large scale bone defects, also known as megaprostheses are one of the most widely used treatments. 300+ explants were collected from several hospitals from the past 20 years. From this set, 37 hinge knee megaprostheses from Stryker, Zimmer, Biomet, and Depuy were retrieved and the corresponding patient operative notes, radiographs, and post-replacement implant images were examined. Revision reasons, standarized reasons, XRF data, age, sex, material, cementation, implantation time, interface scoring, and many other parameters were looked at extensively. Explants were all then analyzed in order to determine the common causes for failure and revision experienced by many patients. Our complete findings will better inform implant manufacturers when creating future megaprostheses.
STAR student: Lex Stowe Fused filament fabrication (FFF) is the process in which thermoplastics are heated and deposited in a layer-by-layer method to create objects. There are many different types of filaments that are used for this manufacturing process, with the leader in strength being carbon fiber reinforced filament. These filaments have strands of carbon fiber oriented parallelwithin the thermoplastic to increase physical and thermal properties of the material. Our study focused on the mechancial properties of these reinforced filaments, with a specific interest in carbon fiber acrylonitrile butadiene styrene (CF-ABS) We tested the mechanical propereties of CF-ABS when printed in the XY, XZ, and YZ directions, and when printed at certain parameters. Such parameters include specific nozzle diameters, extrusion multipliers, and layer heights. Tensile strength specimens were constructed according to ASTM standards and were sliced in each of the directions. These specimens were tested, then imaged by an SEM to review fiber orientation after printing, as well as the breaking point of the specimen.
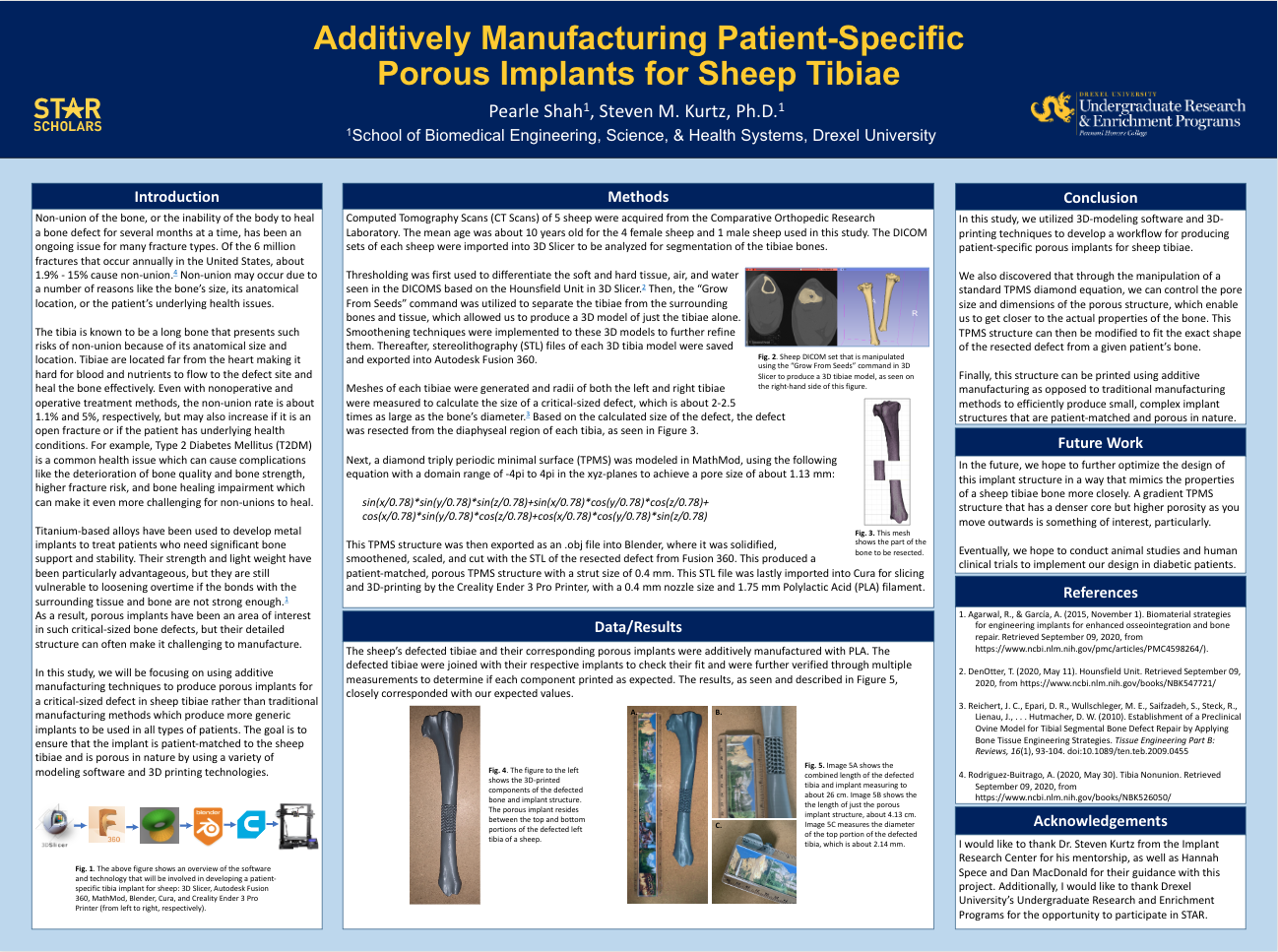
STAR student: Pearle Shah Of the 6 million fractures that occur annually in the U.S., about 1.9% - 15% cause non-union, which is the body's inability to heal a bone defect for several months at a time. Factors such as the bone's size, anatomical location, or the patient's underlying health issues can influence non-union. The development of porous structures can be useful in promoting the healing of such defected bones; however, they can be challenging to incorporate in implant using traditional manufacturing methods due to their complexity and size. In order to achieve such structures in an implant, a sheep DICOM set was used to generate a 3D model of the tibae which allowed for a critical sized defect to be resected from the bone. Then, MathMod and Blender were utilized to generate a diamon triply periodic minimal surface in the shape of the resected bone. This structure was then sliced and 3D printed to produce a fully porous implant that was patient-specific for the sheep tibia. This workflow will be particularly useful in producing implant structures that closely mimic the properties of a patient's bone while also be patient specific. Future work will include optimizing the design of this implant before animal trials are conducted.