Chapter 3. Ceramic-on-Ceramic Bearings in Primary THA
Steven M. Kurtz, PhD.
Jump to a Section
3.1 Introduction
3.2 Alumina-Alumina COC Bearings with Traditional Modular Liners.
3.3 Delta-Delta COC Bearings with Traditional Modular Liners
3.4 Large-Diameter Monoblock Cups for Delta-Delta COC Bearings
3.5 Survivorship of COC Bearings in International Registries
3.6 Do COC Bearings Mitigate Dislocation?
3.7 Summary
3.8 Acknowledgements
3.9 References
3.1 Introduction
Contemporary ceramic-on-ceramic (COC) bearings are regarded today as exhibiting the lowest wearing articulating surfaces in hip arthroplasty. Indeed, the long-term clinical literature supports COC as having significantly lower (undetectable) wear when compared with historical and conventional, non highly crosslinked polyethylene available up to the mid 1990s [48, 49]. In a recent review, Jeffers and Walters [48] wrote, “COC is the only bearing combination that has long-term (10 to 20 years) survival without adverse reaction to wear debris.”
Potential rare concerns related to COC have been realized in the past 40 years related to fracture, squeaking, and disassociation in sandwich ceramic liner designs incorporating polyethylene. As discussed in Chapter 2, the risk of fracture has been reduced to 1/100,000 with the introduction of new alumina matrix composite ceramic materials (e.g., BIOLOX®delta). The risk of squeaking is low and rarely leads to revision. Finally, the risk of sandwich ceramic liner disassociation has been addressed by the community migrating to traditional, taper locking ceramic inserts in a metal shell, as well as by large-diameter monoblock shell designs.
We have already discussed the different types of ceramic biomaterials (Chapter 1) and summarized how ceramic components are manufactured (Chapter 2). There are many published papers dealing with ceramics and hip arthroplasty, and the growth of knowledge in this field is increasing exponentially (Figure 3.1). A search of PubMed in July 2015 using the key words, “ceramics,” “alumina,” “zirconia,” “oxidized zirconium” or “Oxinium” and “hip” yielded over 1,750 articles. Over a third of the published literature on this topic has appeared in the past five years. Thus, a substantial number of scientific articles have emerged dealing with ceramic hip components, and this body of literature is always being continuously updated and expanded.
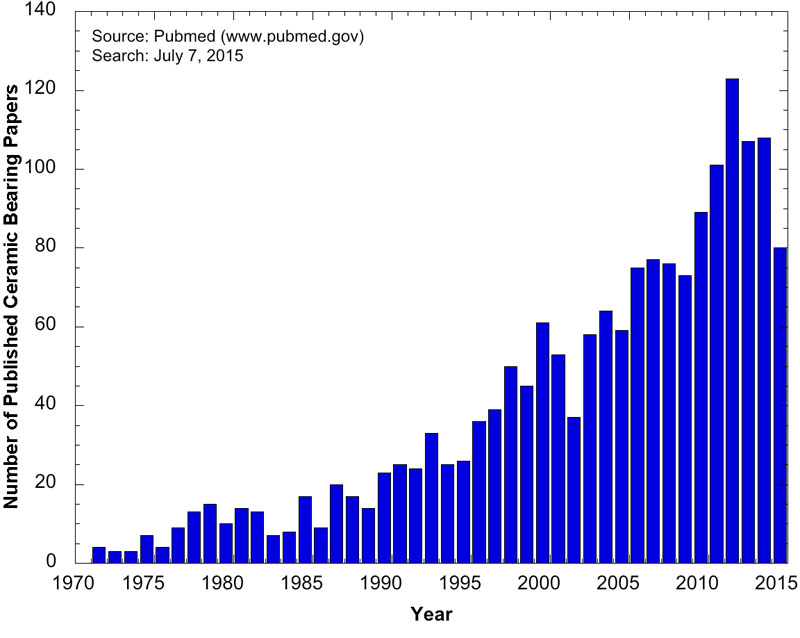
Figure 3.1.The number of clinical and scientific papers on ceramic bearings is increasing exponentially over time. The advanced Pubmed (www.pubmed.gov) search syntax used to generate this figure was: (((ceramic OR alumina OR zirconia OR oxidized zirconium OR Oxinium)) AND hip). The search includes publications up to and including July 7, 2015.
In this chapter we will focus on synthesizing the literature as it pertains to the outcomes of ceramic-on-ceramic (COC) bearings in primary total hip arthroplasty (THA). If the reader is interested in literature about the use of ceramic bearings in revision surgery, you should skip ahead to Chapter 4.
^ Return to Top
3.2 Alumina-Alumina COC Bearings with Traditional Modular Liners
In a comprehensive, systematic review of alumina COC hips literature [48], Jeffers and Walters provided an overview of the clinical performance of ceramic bearings published up to 2011. For this chapter, the systematic search of the scientific and clinical literature (described in Section 3.1) identified 10 studies with 10 or more years of clinical follow-up for traditional taper locking alumina liner designs (Table 3.1). Of these 10 long-term alumina COC studies, only four were previously available at the time of Jeffers and Walters’ review [48]. It is clear from Table 3.1 that the rates of long-term dislocation (0-3.6%); aseptic loosening (0-4.8%); and survivorship (95.2-99% at 10+ years); demonstrate the long-term safety and effectiveness of alumina COC bearings in primary THA using traditional taper lock liner designs.
Table 3.1.Summary of long-term clinical outcomes, on average 10 years or more follow-up, reported for alumina COC total hip replacements. These studies all included a traditional, taper locking ceramic insert in a metal shell. Adapted in part from Jeffers and Walter [48].
| Study | Cup Manufacturer Design | Number of Hips | Mean follow-up in years (range) | Dislocation(%) | Aseptic Loosening (%) | Kaplan Meier Survival |
| Boyer et al. [50] | Ceraver Osteal | 83 | 10 (7 to 15) | 3.6 | 4.8 | - |
| Kim et al. [51] | DePuy Duraloc | 102 | 11 (10 to 13) | 2.0 | 0 | 99% at 11 years |
| Kress et al. [52] | Ceraver Osteal Cerafit | 75 | 11 (10 to 11) | - | 0 | - |
| Lee et al. [53] | Aesculap Plasmacup | 100 | > 10 | 1.0 | 0 | 97% at 11 years |
| D’Antonio et al. [54] | Stryker ABC | 194 | 10.3 (>10) | 0.5 | 0 | 95.2 - 97.9% at 10 years |
| D’Antonio et al. [55] | Stryker Trident | 209 | > 10 | 1 | 0.5 | 97% at 10 years |
| Sugano et al. [56] | Cremascoli, AnCA | 100 | 12.4 (11 to 14) | - | 0 | 97.6% at 14 years |
| Solarino et al. [57] | Ceraver Osteal Triradius-M | 68 | 12.9 (11 to 15) | 0 | 0 | 97.0% at 13 years |
| Vendittoli et al. [49] | Ceraver Osteal Cerafit | 71 | 12.3 (9 to 15) | 0 | 1.4 | 98.6% at 15 years |
| Kang et al. [58] | Aesculap Plasmacup | 90 | (14 to 16) | 2.2 | 0 | 98.9% at 15.9 years |
The foundation of contemporary COC total hips rests on the successful clinical performance of alumina bearings. Although clearly successful (Table 3.1), alumina COC bearings are limited to head sizes, in order to safely accommodate the traditional taper locking ceramic liner design. In recent years, a combination of ceramic material and design changes has been introduced to safely accommodate head sizes of 36 mm or greater (Chapter 2). Here, we now focus on the clinical evidence for bearings incorporating alumina matrix composites (i.e., BIOLOX®delta). Clinical studies refer to these new COC bearings as “delta COC” [59, 60]. We will maintain this nomenclature here. Although we will first summarize the literature for delta COC in the context of traditional modular liners, we will also discuss the clinical performance of large-diameter COC bearings with monoblock acetabular cups. Finally, we summarize the growing evidence that COC bearings influence the risk of hip dislocation in primary THA.
^ Return to Top
3.3 Delta-Delta COC Bearings with Traditional Modular Liners
From our systematic search of the literature (described in Section 3.1), we identified six unique clinical studies describing the clinical performance of delta COC bearings with up to 6 years of follow-up (Table 3.2). We did not include short-term reports when longer-term follow-up of the same patient population was available. These independent studies all included cementless, modular acetabular components with a traditional taper locking BIOLOX®delta insert. The maximum head size used in these studies was 36 mm. As summarized in Table 3.2, the Kaplan Meier survivorship at 5 to 6 years of follow-up ranged between 96.9% and 98.5%. The six studies identified by our systematic review are summarized below.
Table 3.2.Summary of clinical outcomes reported for delta COC total hip replacements. These studies all included a traditional, taper locking ceramic insert in a cementless metal shell.
| Study | Cup Design, Manufacturer | Head Size | Number of Hips | Mean follow-up in years | Dislocation (%) | Kaplan Meier Survival |
| Baek et al. [61] | Bencox, CorenTec | 32 and 36 mm | 91 | 5 | 1.1% | 97.9% at 5 years |
| Hamilton et al. [59] | Pinnacle, DePuy Synthes | 28 and 36 mm | 345 | > 5 | 3.2% for 28 mm; 1.8% for 36 mm | 96.9% at 6 years |
| Shin et al. [62] | Plasmacup, Aesculap | 36 mm | 83 | 2 | 3.7% | - |
| Aoude et al. [63] | Pinnacle, DePuy Synthes | 28 and 36 mm | 133 | 6 (3.3 - 9.4) | 0.8% | 98.5% at 6 years |
| Wang et al. [64] | Pinnacle, DePuy Synthes | 32 and 36 mm | 177 | 2 (1-5) | 1.1% | - |
| Cai et al. [60] | Beta, Link Medical Technology | 36 mm | 51 | 3.3 (3-3.7) | 1.9% | - |
Hamilton and colleagues [59] have published the mid-term results of two Investigational Device Exemption (IDE) studies performed for the U.S. Food and Drug Administration. Together, the two combined U.S. studies comprise the largest body of scientific data available today for delta COC bearings with 28 and 36 mm diameter femoral heads. The mean patient age was 56 to 57 years. A Pinnacle cup (Depuy Synthes) was implanted in 345 delta COC hips between 2003 and 2007. Revisions were performed for infection (n=3), stem loosening (n=4), and liner fracture (n=2). There were nine dislocations and three post-operative liner fractures; one of these patients with a fractured liner refused to be revised. Squeaking was reported by 26 of the 345 patients (7.5%). However, only one patient could actually reproduce the reported sounds during an office visit, and none were revised or asked to be revised due to squeaking.
Aoude et al. [63] from Montreal Canada evaluated 115 patients (133 hips) who received a delta COC Pinnacle cup (DePuy Synthes) between 2004 and 2010. The patients were less than 65 years old (mean 43.6y, range: 14-65y). A 36 mm femoral head was used in 74% of the cases; the remainder received a 28 mm head. Two patients were revised for infection and instability, respectively. A female patient with a 36 mm head developed squeaking after a fall. She was pain free and refused to be revised.
Shin and colleagues [62] prospectively studied 83 patients from South Korea who received a delta COC bearing with a 36 mm diameter femoral head between 2010 and 2012 (Plasmacup, Aesculap). One group of patients (n=22; mean age, 57 years) received a factory preassembled acetabular component in which the liner was fitted to the shell; the second group of patients received a traditional modular liner (n=61; mean age, 61 years). The radiographic and functional outcomes were the same in both groups after two years of follow-up. Post-operative complications included 3 patients who suffered from early dislocation and were treated by closed reduction. No ceramic fractures or revisions were reported. The authors found that a factory-preassembled liner was an attractive option for female patients with a small acetabulum, allowing them to more frequently accommodate a 36 mm femoral head size.
Baek et al. [61] from South Korea studied 94 delta COC hips in 91 patients (mean age, 55 years) who were implanted with a Bencox cup (CorenTec) by a single surgeon in 2009. Patients were followed for five years. Three reported asymptomatic bearing noise (clicking only, no squeaking). One patient dislocated and was treated by closed reduction. There were two revisions, one for periprosthetic fracture and one for liner disassociation. There were no ceramic fractures.
Wang and colleagues [64] from Beijing China followed 177 delta COC hips in 132 patients (mean age, 42 years) for 2 years on average. All received a Pinnacle cup (DePuy Synthes) and a 32 mm (n=37/177) or 36 mm femoral head (n=140/177) between 2010 and 2012. Two patients dislocated and were treated by closed reduction. Two patients reported asymptomatic squeaking. Two patients were revised, one because of liner fracture, one due to femoral fracture.
Cai et al. [60] performed a prospective randomized trial in Hunan China comparing delta COC bearings with alumina ceramic on conventional polyethylene hips. We summarized the findings from the delta COC cohort, which included 51 hips in 43 patients (mean age, 42 years) who were followed for 3.6 years, on average. The surgeries were performed in 2008 using implants manufactured by Link. Intraoperative chipping occurred with one delta liner. Postoperatively, two patients were revised due to recurring dislocation and infection, respectively. Two patients reported component related noise.
Overall, the available published international clinical studies indicate that delta COC is a safe and reliable bearing combination at short and intermediate time points. Acceptably low rates of fracture and squeaking were reported in these studies, consistent with the expectations of the investigators. While encouraging, investigations are still needed with long-term follow-up, so that after 10 years in vivo, results may be compared with the gold standard alumina COC THAs.
^ Return to Top
3.4 Large-Diameter Monoblock Cups for Delta-Delta COC Bearings
Comparatively few studies describe the clinical performance of delta COC bearings for head sizes larger than 40 mm. These new monoblock cup designs, described in Chapter 2, such as DELTAMOTION® (DePuy Synthes) are currently only available outside the U.S. and thusfar only two short-term studies have been published with around 2 years of follow-up. Both studies have focused on reports of squeaking in this new delta COC design, which has head diameters of up to 48 mm, depending upon the outer diameter of the cup.
In the study by McDonnell and colleagues [65] from the UK, investigators studied 208 patients with a mean age of 59 years. Between 2009 and 2011, the patients received a DELTAMOTION® cup and one of four types of cementless stems manufactured by either Finsbury or DePuy. Patients were followed for 21 months (12 to 35). 65 patients (31%) reported bearing noise, of which 43/65 reported squeaking. When they analyzed which factors helped explain squeaking, they found significantly greater hip laxity and smaller femoral component sizes among squeaking patients as compared to those with silent bearings. The authors reported that, “All patients were satisfied with their THR, and none of those with squeaking hips were concerned or wanted further surgery” [65]. There were no revisions. One patient dislocated and was successfully treated with a closed reduction.
During a similar study conducted in Australia, Tai et al. [66] followed 206 DELTAMOTION® cases for 28 months on average. The authors used a Securefit uncemented femoral stem in all cases (Stryker). Upon radiographic review, the authors judged that all of the delta cups had bony ingrowth. Asymptomatic or benign squeaking was reported for 15 hips (7.3%) but was not associated with cup position. There was one pulmonary embolism, one dislocation, two periprosthetic fractures, and two subsided stems in this study. The dislocation case and the two periprosthetic fracture cases, all attributed to trauma, were revised. The authors surmised that the lower rate of squeaking in their series, as compared with the previous study by McDonnell [65], may have been related to differences in the design, flexibility, and sizing of stems by the two groups of investigators.
Further studies are needed to determine if these new large diameter COC designs continue their successful track record at intermediate and long-term follow-up periods. Additional data regarding these large-diameter COC bearings can be found in international registries and are summarized in the following section.
^ Return to Top
3.5 Survivorship of COC Bearings in International Registries
As we have seen in the previous sections, many studies document the long-term survivorship of alumina COC bearings and, at intermediate time points, for delta COC ceramics. As a general class of hip implants, the 2014 reports from both the Australian registry [6] and NJR from the UK [1] provide additional long-term data on COC survivorship, which compares favorably to the values published in the literature. There is also short-term data on delta COC bearings in the Australian registry reports.
COC hips the second most frequently reported type of articulating surface in the Australian registry [6]. The Australian registry treats COC as a general class and, for the first time in 2014, also provided a breakdown based on the type of ceramic [6]. Overall, the crude (unadjusted) revision rate of 57,828 primary COC THAs in Australia was 5.2% (95% CI: 4.9, 5.5) at 10 years, corresponding to a 10-year survivorship of 94.8% across all implant designs, manufacturers, surgeons, and patients. The registry reported that head size was an important predictor for clinical outcome, with 28 mm heads having the highest 10-year revision rate (6.6%; 95% CI: 6.0, 7.3) among COC bearings. The revision rate of 32 mm COC bearings at 10 years was significantly lower (4.8%; 95% CI: 4.4, 5.2), and comparable to 36-38 mm bearings at 10 years (5.3%; 95% CI: 4.6, 6.1). There was a slight but significant difference in outcome of COC by fixation type, with hybrid hips having a lower rate (4.7%; 95% CI: 4.0, 5.5) than cementless hips (5.3%; 95% CI: 5.0, 5.6) at 10 years.
Outcomes for the large-diameter (40 mm) delta COC bearings were only available for 3 years follow-up in the 2014 Australian registry [6]. The cumulate revision rate of 1.8% (CI: 1.4, 2.3) at 3 years was considered to be “satisfactory” for the short time period.
In the UK, COC hips gained popularity after MOM bearings fell out of favor [1]. By 2011, about 45% of uncemented hips in the NJR incorporated a COC bearing. In the 2014 report, 98,653 patients with a COC hip were registered by the NJR favor [1]. Results are only tabulated by 2 fixation types: uncemented or hybrid fixation (with an uncemented acetabulum and cemented stem); there are no cases of cemented or reverse hybrid fixation reported for COC in the NJR. Overall, the crude (unadjusted) revision rate of 81,205 primary uncemented COC THAs was 4.75% (95% CI: 4.11-5.47) at 10 years. For 17,448 primary COC THAs with hybrid fixation, the 10-year revision rate was 2.80% (95% CI: 2.16-3.63). No statistical comparisons were made between groups for fixation type. The report does not include details about head size or ceramic material used in COC.
Taken together, the Australian and UK registries show comparable long-term outcomes for COC bearings [1, 6], with approximately 95% survivorship in both countries at 10-years of follow-up. As we noted in our summary of the registry outcomes for COP (Section 3.2.3), these data as presented in the annual reports are limited and comparisons must be interpreted with caution. Although the Australian registry attempts some statistical adjustment for bearing effects by age and gender, these basic adjustments are not applied to the bearing data in the 2014 UK annual report. Despite these limitations, the available registry data does independently demonstrate the successful long-term clinical performance of COC bearings in a variety of hip implant designs and across different nations and large patient populations.
^ Return to Top
3.6 Do COC Bearings Mitigate Dislocation?
Few studies have examined the role of COC bearings in dislocation [67-72]. Researchers from California, USA, followed their alumina COC patients (with traditional modular cup designs manufactured by Stryker) between 1997 and 2005 out of concern that the limited neck length and head sizes that were available at the time might pose a greater risk of dislocation [67, 68]. In a single center series of 336 COC hips [68] implanted using a posterolateral approach with capsular repair, researchers observed only 2 early dislocations (within one year of surgery) that were treated with closed reduction. They reported no fractures or revisions within their 8-year follow-up period. In a larger multicenter study with 1,635 patients followed for up to 7 years (2.9 years, on average) with alumina COC (Stryker), researchers observed an overall dislocation rate of 1.1% between 1996 and 2005 [67]. Taken together, these observational studies [67, 68] both found that contemporary alumina COC hips have an acceptably low dislocation rate.
Interest that bearings might serve as a potential mitigating factor for dislocation was first raised by researchers from France who, at long-term follow-up, observed fewer late dislocations, less tissue damage, and better preserved hip musculature around the hips of patients implanted with COC as opposed to C-PE [69, 70]. Hernigou and colleagues [69] implanted 252 hips in 126 patients with a COC bearing on one side and a C-PE bearing on the contralateral side. The surgeries were performed between 1978 and 1985 using 32 mm diameter, cemented alumina or polyethylene sockets (Ceraver) with up to 34 years follow-up. In the C-PE group, the risk of dislocation was 2% at year 1, and increased to 13% at 30 years; by contrast only 2% of COC patients were revised for dislocation within 30 years, and these revisions occurred within the first two years. Thus, the two types of hips had the same risk of short-term dislocation, but the long-term risk was significantly greater in the C-PE hips as compared with the COC hips. At the time of revision, the C-PE had greater histological changes than the COC group, leading the investigators to hypothesize that the polyethylene particles were compromising the soft tissue around the hip joint, and contributing to greater risk of late dislocation. They also postulated that increased wear of the polyethylene might contribute to dislocation, by tunneling in of the head into the socket and increasing the risk of impingement and levering out of the socket. These findings are noteworthy given the historical context in which the implants were installed (prior to 1985), which must be remembered was at a time of gamma sterilization in air for polyethylene, over a decade before the development of highly crosslinked polyethylene (HXLPE). There can be little doubt that 32 mm diameter, gamma air sterilized polyethylene sockets, available to clinicians in the 1980s, would be susceptible to much greater volumetric wear than COC hips and, concomitant periprosthetic inflammation. It is also known, however, that modern HXLPEs have greatly reduced the wear and risk of osteolysis in today’s hip replacements [73] so it is unclear how to apply the findings of Hernigou and colleagues [69, 70] to modern implants and surgical techniques.
Dislocation risk depends upon a variety of factors, both surgical, patient, and design. Tsukada et al. [72] investigated the dislocation risk of COC hips based on the surgical approach. The authors followed a consecutive series of 139 THAs via the direct anterior approach (DAA) from 2000-2006 with 177 THAs via posterior approach (PA) from 2006-2009. The modular Plasmacup design was used with an alumina insert (Aesculap) with 28 and/or 32 mm heads. The PA cohort as treated using 28 mm heads, whereas the DAA cohort received a combination of 28 mm (n=85) and 32 mm heads (n=54). There were no dislocations in the DAA group and 7 dislocations in the PA group (4%). Although there was some confounding with head size, the authors attributed the DAA surgical approach for the lower dislocation rate in that group of patients.
Pitto and colleagues [71] studied the effect of bearing surface on dislocation risk using the New Zealand Registry and national data for primary THA between 1999 and 2012. Among the 81,972 primary THAs, 10% were COC, 17% were C-PE, 0.5% were ceramic on metal, 7% were MOM, and 65% were MOP. They used Cox regression to adjust for the following confounding factors: patient age, surgical approach, and head size. After adjustment, they found no significant reduction of dislocations in the COC cohort (p=0.09). The authors did not discuss the gradual introduction of HXLPE over this time period as a potential confounding factor in their analysis.
The Australian and UK registries provide additional comparative data for the dislocation rates of COC as compared with C-PE and M-PE bearings. Although the latest UK registry report, from 2014, contains comparative data for the revision rate due to dislocation for different bearing materials, these raw data are unadjusted and presented without statistical analysis [1]. In the 2014 report of the Australian registry [6], a significant difference in revision due to dislocation was noted for head sizes ≥ 38 mm (see Table D7 in the 2014 report). There was no difference in revision for dislocation with head sizes ≤ 36 mm. A study by Sexton and colleagues [74], using earlier Australian registry data up to 2007, found that COC bearings had no significant effect on dislocation risk when adjusting for patient age and head size. Sexton’s analysis published in 2009 did not account for surgical approach, and the data in their study preceded the introduction of head sizes ≤ 38 mm [74].
In summary, whether COC bearings reduce long-term dislocation risk is a controversial topic in the literature, and is complicated by differences in head size, surgical approach, and polyethylene bearing materials over the years. Evidence in support of this hypothesis is largely based on C-PE hips in which historical, gamma air sterilized polyethylene was used [69]. In that study, there was no evidence that COC bearings implanted the 1980s improved short-term dislocation risk; only the long-term dislocation risk was improved for the COC cohort because of the relative inertness of low volume of ceramic wear debris compared to gamma air sterilized polyethylene. Today, there is little evidence that, with modern bearing materials including HXLPE, COC bearings will offer a substantial further advantage in dislocation risk over other contemporary M-PE or C-PE bearings. Only longer-term studies will be able to determine if the COC offers a dislocation benefit after 20 or more years of implantation.
^ Return to Top
3.7 Summary
Today, COC is currently one of the most well-established, “mainstream” alternative bearings and incorporates the successful elements of historical precedents. Ceramic bearings, used in over ten million patients worldwide [89], are increasingly indicated for patients with a long life expectancy. As we previously explained in Chapter 2, the use of ceramic bearings does entail potential risks for the patient, however these risks are today considered to be acceptably low by the clinical community. In the following chapter we will review the clinical evidence for ceramic-on-polyethylene bearings.
3.8 Acknowledgements
The author would like to thank Christina Arnholt, Drexel University, for her editorial assistance with this chapter.
^ Return to Top
3.9 References for Chapter 3
[1] National Joint Registry for England and Wales. 11th Annual NJR Report. London: NJR; 2014. [2] Lancaster JG, Dowson D, Isaac GH, Fisher J. The wear of ultra-high molecular weight polyethylene sliding on metallic and ceramic counterfaces representative of current femoral surfaces in joint replacement. Proceedings of the Institution of Mechanical Engineers. 1997;211:17-24. [3] Cuckler JM, Bearcroft J, Asgian CM. Femoral head technologies to reduce polyethylene wear in total hip arthroplasty. Clin Orthop. 1995;317:57-63. [4] Meftah M, Klingenstein GG, Yun RJ, Ranawat AS, Ranawat CS. Long-term performance of ceramic and metal femoral heads on conventional polyethylene in young and active patients: a matched-pair analysis. J Bone Joint Surg Am. 2013;95:1193-7. [5] Wang S, Zhang S, Zhao Y. A comparison of polyethylene wear between cobalt-chrome ball heads and alumina ball heads after total hip arthroplasty: a 10-year follow-up. J Orthop Surg Res. 2013;8:20. [6] Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA; 2014. [7] Agency for Healthcare Research and Quality. Nationwide Inpatient Sample. [8] Sugano N, Nishii T, Nakata K, Masuhara K, Takaoka K. Polyethylene sockets and alumina ceramic heads in cemented total hip arthroplasty. A ten-year study. J Bone Joint Surg Br. 1995;77:548-56. [9] Cales B. Zirconia as a sliding material: histologic, laboratory, and clinical data. Clin Orthop. 2000;379:94-112. [10] Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649-61. [11] Kim YH. Comparison of polyethylene wear associated with cobalt-chromium and zirconia heads after total hip replacement. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:1769-76. [12] Kraay MJ, Thomas RD, Rimnac CM, Fitzgerald SJ, Goldberg VM. Zirconia versus Co-Cr femoral heads in total hip arthroplasty: early assessment of wear. Clin Orthop Relat Res. 2006;453:86-90. [13] Hernigou P, Bahrami T. Zirconia and alumina ceramics in comparison with stainless-steel heads. Polyethylene wear after a minimum ten-year follow-up. J Bone Joint Surg Br. 2003;85:504-9. [14] Sychterz CJ, Engh CA, Jr., Young AM, Hopper RH, Jr., Engh CA. Comparison of in vivo wear between polyethylene liners articulating with ceramic and cobalt-chrome femoral heads. J Bone Joint Surg Br. 2000;82:948-51. [15] Hendrich C, Goebel S, Roller C, Kirschner S, Martell JM. Wear performance of 28 millimeter femoral heads with the Harris-Galante cup: Comparison of alumina and cobalt chrome. In: Zippel H, Dietrich M, editors. Bioceramics in Joint Arthroplasty, 8th Biolox Symposium Proceedings. Darmstadt: Steinkopff Verlag; 2003. p. 177-82. [16] Hopper RH, Jr., Engh CA, Jr., Fowlkes LB, Engh CA. The pros and cons of polyethylene sterilization with gamma irradiation. Clin Orthop Relat Res. 2004:54-62. [17] Hopper RH, Jr. Personal communication. AORI; 2008. [18] Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, Miller RK. Ceramic-on-polyethylene bearing surfaces in total hip arthroplasty. Seventeen to twenty-one-year results. J Bone Joint Surg Am. 2001;83-a:1688-94. [19] Ihle M, Mai S, Siebert W. Ceramic versus metal femoral heads in combination with polyethylene cups: Long-term wear analysis at 20 years. Semin Ortho. 2011;22:218-24. [20] Wroblewski BM, Siney PD, Dowson D, Collins SN. Prospective clinical and joint simulator studies of a new total hip arthroplasty using alumina ceramic heads and cross-linked polyethylene cups. Journal of Bone & Joint Surgery. 1996;78 B:280-5. [21] Wroblewski BM, Siney PD, Fleming PA. Low-friction arthroplasty of the hip using alumina ceramic and cross-linked polyethylene. A 17-year follow-up report. J Bone Joint Surg Br. 2005;87:1220-1. [22] Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop. 1970;72:7-21. [23] Kim YH, Kim JS, Choi YW, Kwon OR. Intermediate results of simultaneous alumina-on-alumina bearing and alumina-on-highly cross-linked polyethylene bearing total hip arthroplasties. J Arthroplasty. 2009;24:885-91. [24] Oonishi H, Kim SC, Takao Y, Kyomoto M, Iwamoto M, Ueno M. Wear of highly cross-linked polyethylene acetabular cup in Japan. The Journal of arthroplasty. 2006;21:944-9. [25] Nakahara I, Nakamura N, Nishii T, Miki H, Sakai T, Sugano N. Minimum Five-Year Follow-Up Wear Measurement of Longevity Highly Cross-Linked Polyethylene Cup Against Cobalt-Chromium or Zirconia Heads. J Arthroplasty. 2009. [26] Ise K, Kawanabe K, Tamura J, Akiyama H, Goto K, Nakamura T. Clinical results of the wear performance of cross-linked polyethylene in total hip arthroplasty: prospective randomized trial. The Journal of arthroplasty. 2009;24:1216-20. [27] Kawate K, Ohmura T, Kawahara I, Tamai K, Ueha T, Takemura K. Differences in highly cross-linked polyethylene wear between zirconia and cobalt-chromium femoral heads in Japanese patients: a prospective, randomized study. The Journal of arthroplasty. 2009;24:1221-4. [28] Meftah M, Ebrahimpour PB, He C, Ranawat AS, Ranawat CS. Preliminary clinical and radiographic results of large ceramic heads on highly cross-linked polyethylene. Orthopedics. 2011;34:133. [29] Kim YH, Park JW, Kulkarni SS, Kim YH. A randomised prospective evaluation of ceramic-on-ceramic and ceramic-on-highly cross-linked polyethylene bearings in the same patients with primary cementless total hip arthroplasty. International orthopaedics. 2013;37:2131-7. [30] Epinette JA, Manley MT. No differences found in bearing related hip survivorship at 10-12 years follow-up between patients with ceramic on highly cross-linked polyethylene bearings compared to patients with ceramic on ceramic bearings. J Arthroplasty. 2014;29:1369-72. [31] Wyles CC, Jimenez-Almonte JH, Murad MH, Norambuena-Morales GA, Cabanela ME, Sierra RJ, Trousdale RT. There Are No Differences in Short- to Mid-term Survivorship Among Total Hip-bearing Surface Options: A Network Meta-analysis. Clin Orthop Relat Res. 2015;473:2031-41. [32] Kurtz SM, Kocagoz SB, Hanzlik JA, Underwood RJ, Gilbert JL, Macdonald DW, Lee GC, Mont MA, Kraay MJ, Klein GR, Parvizi J, Rimnac CM. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471:3270-82. [33] Black J. Does Corrosion Matter? The Journal of Bone & Joint Surgery1988. p. 517-20. [34] Collier JP, Surprenant VA, Jensen RE, Mayor MB. Corrosion at the interface of cobalt-alloy heads on titanium-alloy stems. Clin Orthop Relat Res. 1991:305-12. [35] Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res. 1993;27:1533-44. [36] Gilbert JL, Jacobs JJ. The mechanical and electrochemical processes associated with taper fretting crevice corrosion: a review. In: Marlowe D, Parr J, Mayor MB, editors. Modularity of Orthopedic Implants. Conshohocken, PA: ASTM; 1997. p. 45-59. [37] Urban RM, Jacobs JJ, Gilbert JL, Rice SB, Jasty M, Bragdon CR, Galante JO. Characterization of solid products of corrosion generated by modular-head femoral stems of different designs and materials, STP 1301. In: Marlowe D, Parr J, Mayor MB, editors. Modularity of Orthopedic Implants. Conshohocken, PA: ASTM; 1997. p. 33-44. [38] Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80:268-82. [39] Langton DJ, Sidaginamale R, Lord JK, Nargol AV, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings. Bone & Joint Research - Hip. 2012;1:56-63. [40] Langton DJ, Jameson SS, Joyce TJ, Gandhi JN, Sidaginamale R, Mereddy P, Lord J, Nargol AV. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br. 2011;93:1011-6. [41] Gill IP, Webb J, Sloan K, Beaver RJ. Corrosion at the neck-stem junction as a cause of metal ion release and pseudotumour formation. J Bone Joint Surg Br. 2012;94:895-900. [42] Cooper HJ, Della Valle C, Berger RA, Tetreault BA, Paprosky W, Sporer S, Jacobs JJ. Corrosion at the Head-Neck Taper as a Cause for Adverse Local Tissue Reactions After Total Hip Arthroplasty. Journal of Bone and Joint Surgery, Am. 2012;94:1655 - 61. [43] Urban RM, Jacobs JJ, Gilbert JL, Galante JO. Migration of corrosion products from modular hip prostheses. Particle microanalysis and histopathological findings. J Bone Joint Surg Am. 1994;76:1345-59. [44] Jacobs JJ, Urban RM, Gilbert JL, Skipor AK, Black J, Jasty M, Galante JO. Local and distant products from modularity. Clin Orthop Relat Res. 1995:94-105. [45] Hallab NJ, Messina C, Skipor A, Jacobs JJ. Differences in the fretting corrosion of metal-metal and ceramic-metal modular junctions of total hip replacements. J Orthop Res. 2004;22:250-9. [46] Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, Leurgans S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002:149-61. [47] Kocagoz SB, Underwood RJ, MacDonald D, Gilbert JL, Rimnac CM, Kurtz SM. Metal release in ceramic and CoCr heads at the modular junction: a matched cohort retrieval study. Trans Orthop Res Soc. 2015;Poster Session PS1-065:0887. [48] Jeffers JR, Walter WL. Ceramic-on-ceramic bearings in hip arthroplasty: state of the art and the future. J Bone Joint Surg Br. 2012;94:735-45. [49] Vendittoli PA, Riviere C, Lavigne M, Lavoie P, Alghamdi A, Duval N. Alumina on alumina versus metal on conventional polyethylene: a randomized clinical trial with 9 to 15 years follow-up. Acta orthopaedica Belgica. 2013;79:181-90. [50] Boyer P, Huten D, Loriaut P, Lestrat V, Jeanrot C, Massin P. Is alumina-on-alumina ceramic bearings total hip replacement the right choice in patients younger than 50 years of age? A 7- to 15-year follow-up study. Orthopaedics & traumatology, surgery & research : OTSR. 2010;96:616-22. [51] Kim YH, Choi Y, Kim JS. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head osteonecrosis. International orthopaedics. 2010;34:1123-7. [52] Kress AM, Schmidt R, Holzwarth U, Forst R, Mueller LA. Excellent results with cementless total hip arthroplasty and alumina-on-alumina pairing: minimum ten-year follow-up. International orthopaedics. 2011;35:195-200. [53] Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. The Journal of bone and joint surgery American volume. 2010;92:1715-9. [54] D'Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470:373-81. [55] D'Antonio JA, Capello WN, Naughton M. High survivorship with a titanium-encased alumina ceramic bearing for total hip arthroplasty. Clin Orthop Relat Res. 2014;472:611-6. [56] Sugano N, Takao M, Sakai T, Nishii T, Miki H, Ohzono K. Eleven- to 14-year follow-up results of cementless total hip arthroplasty using a third-generation alumina ceramic-on-ceramic bearing. J Arthroplasty. 2012;27:736-41. [57] Solarino G, Piazzolla A, Notarnicola A, Moretti L, Tafuri S, De Giorgi S, Moretti B. Long-term results of 32-mm alumina-on-alumina THA for avascular necrosis of the femoral head. J Orthop Traumatol. 2012;13:21-7. [58] Kang BJ, Ha YC, Ham DW, Hwang SC, Lee YK, Koo KH. Third-generation alumina-on-alumina total hip arthroplasty: 14 to 16-year follow-up study. J Arthroplasty. 2015;30:411-5. [59] Hamilton WG, McAuley JP, Blumenfeld TJ, Lesko JP, Himden SE, Dennis DA. Midterm Results of Delta Ceramic-on-Ceramic Total Hip Arthroplasty. J Arthroplasty. 2015. [60] Cai P, Hu Y, Xie J. Large-diameter Delta ceramic-on-ceramic versus common-sized ceramic-on-polyethylene bearings in THA. Orthopedics. 2012;35:e1307-13. [61] Baek SH, Kim WK, Kim JY, Kim SY. Do Alumina Matrix Composite Bearings Decrease Hip Noises and Bearing Fractures at a Minimum of 5 Years After THA? Clin Orthop Relat Res. 2015. [62] Shin YS, Han SB, Jung TW. Comparison between preassembled and modular cups in primary cementless total hip arthroplasty: a two-year minimum follow-up study. J Arthroplasty. 2014;29:2378-82. [63] Aoude AA, Antoniou J, Epure LM, Huk OL, Zukor DJ, Tanzer M. Midterm Outcomes of the Recently FDA Approved Ceramic on Ceramic Bearing in Total Hip Arthroplasty Patients Under 65Years of Age. J Arthroplasty. 2015;30:1388-92. [64] Wang W, Guo W, Yue D, Shi Z, Zhang N, Liu Z, Sun W, Wang B, Li Z. Fourth-generation ceramic-on-ceramic total hip arthroplasty in patients of 55 years or younger: short-term results and complications analysis. Chin Med J (Engl). 2014;127:2310-5. [65] McDonnell SM, Boyce G, Bare J, Young D, Shimmin AJ. The incidence of noise generation arising from the large-diameter Delta Motion ceramic total hip bearing. The bone & joint journal. 2013;95-B:160-5. [66] Tai SM, Munir S, Walter WL, Pearce SJ, Walter WK, Zicat BA. Squeaking in Large Diameter Ceramic-on-Ceramic Bearings in Total Hip Arthroplasty. J Arthroplasty. 2015;30:282-5. [67] Colwell CW, Jr., Hozack WJ, Mesko JW, D'Antonio JA, Bierbaum BE, Capello WN, Jaffe WL, Mai KT. Ceramic-on-ceramic total hip arthroplasty early dislocation rate. Clin Orthop Relat Res. 2007;465:155-8. [68] Mai K, Hardwick ME, Walker RH, Copp SN, Ezzet KA, Colwell CW, Jr. Early dislocation rate in ceramic-on-ceramic total hip arthroplasty. HSS J. 2008;4:10-3. [69] Hernigou P, Homma Y, Pidet O, Guissou I, Hernigou J. Ceramic-on-ceramic bearing decreases the cumulative long-term risk of dislocation. Clin Orthop Relat Res. 2013;471:3875-82. [70] Hernigou P, Roussignol X, Delambre J, Poignard A, Flouzat-Lachaniette CH. Ceramic-on-ceramic THA Associated With Fewer Dislocations and Less Muscle Degeneration by Preserving Muscle Progenitors. Clin Orthop Relat Res. 2015. [71] Pitto RP, Garland M, Sedel L. Are Ceramic-on-ceramic Bearings in Total Hip Arthroplasty Associated With Reduced Revision Risk for Late Dislocation? Clin Orthop Relat Res. 2015. [72] Tsukada S, Wakui M. Lower Dislocation Rate Following Total Hip Arthroplasty via Direct Anterior Approach than via Posterior Approach: Five-Year-Average Follow-Up Results. The open orthopaedics journal. 2015;9:157-62. [73] Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res. 2011;469:2262-77. [74] Sexton SA, Walter WL, Jackson MP, De Steiger R, Stanford T. Ceramic-on-ceramic bearing surface and risk of revision due to dislocation after primary total hip replacement. J Bone Joint Surg Br. 2009;91:1448-53. [75] Evangelista GT, Fulkerson E, Kummer F, Di Cesare PE. Surface damage to an Oxinium femoral head prosthesis after dislocation. J Bone Joint Surg Br. 2007;89:535-7. [76] Kop AM, Whitewood C, Johnston DJ. Damage of oxinium femoral heads subsequent to hip arthroplasty dislocation three retrieval case studies. J Arthroplasty. 2007;22:775-9. [77] Jaffe WL, Strauss EJ, Cardinale M, Herrera L, Kummer FJ. Surface oxidized zirconium total hip arthroplasty head damage due to closed reduction effects on polyethylene wear. J Arthroplasty. 2009;24:898-902. [78] Mai KT, Verioti C, D'Lima D, Colwell CW, Jr., Ezzet KA, Jr. Surface roughness of femoral head prostheses after dislocation. Am J Orthop (Belle Mead NJ). 2010;39:495-500. [79] McCalden RW, Charron KD, Davidson RD, Teeter MG, Holdsworth DW. Damage of an Oxinium femoral head and polyethylene liner following 'routine' total hip replacement. J Bone Joint Surg Br. 2011;93:409-13. [80] Gibon E, Scemama C, David B, Hamadouche M. Oxinium femoral head damage generated by a metallic foreign body within the polyethylene cup following recurrent dislocation episodes. Orthop Traumatol Surg Res. 2013;99:865-9. [81] Tribe H, Malek S, Stammers J, Ranawat V, Skinner JA. Advanced wear of an Oxinium femoral head implant following polyethylene liner dislocation. Ann R Coll Surg Engl. 2013;95:e133-5. [82] Moussa ME, Esposito CI, Elpers ME, Wright TM, Padgett DE. Hip dislocation increases roughness of oxidized zirconium femoral heads in total hip arthroplasty: an analysis of 59 retrievals. J Arthroplasty. 2015;30:713-7. [83] Garvin KL, Hartman CW, Mangla J, Murdoch N, Martell JM. Wear analysis in THA utilizing oxidized zirconium and crosslinked polyethylene. Clin Orthop Relat Res. 2009;467:141-5. [84] Lewis PM, Moore CA, Olsen M, Schemitsch EH, Waddell JP. Comparison of mid-term clinical outcomes after primary total hip arthroplasty with Oxinium vs cobalt chrome femoral heads. Orthopedics. 2008;31. [85] Morison ZA, Patil S, Khan HA, Bogoch ER, Schemitsch EH, Waddell JP. A randomized controlled trial comparing Oxinium and cobalt-chrome on standard and cross-linked polyethylene. J Arthroplasty. 2014;29:164-8. [86] Garvin KL, White TC, Dusad A, Hartman CW, Martell J. Low Wear Rates Seen in THAs With Highly Crosslinked Polyethylene at 9 to 14 Years in Patients Younger Than Age 50 Years. Clin Orthop Relat Res. 2015. [87] Jassim SS, Patel S, Wardle N, Tahmassebi J, Middleton R, Shardlow DL, Stephen A, Hutchinson J, Haddad FS. Five-year comparison of wear using oxidised zirconium and cobalt-chrome femoral heads in total hip arthroplasty: a multicentre randomised controlled trial. The bone & joint journal. 2015;97-B:883-9. [88] Zaoui A, Hage SE, Langlois J, Scemama C, Courpied JP, Hamadouche M. Do Oxidized Zirconium Femoral Heads Reduce Polyethylene Wear in Cemented THAs? A Blinded Randomized Clinical Trial. Clin Orthop Relat Res. 2015. [89] Heros R. Personal communication. CeramTec; 2015. [90] Dong YL, Li T, Xiao K, Bian YY, Weng XS. Ceramic on Ceramic or Ceramic-on-polyethylene for Total Hip Arthroplasty: A Systemic Review and Meta-analysis of Prospective Randomized Studies. Chin Med J (Engl). 2015;128:1223-31. [91] Si HB, Zeng Y, Cao F, Pei FX, Shen B. Is a ceramic-on-ceramic bearing really superior to ceramic-on-polyethylene for primary total hip arthroplasty? A systematic review and meta-analysis of randomised controlled trials. Hip Int. 2015:0.




