Chapter 5. Ceramic in Revision THA
Steven M. Kurtz, PhD.
Jump to a Section
5.1 Introduction
5.2 Utilization of Ceramic Bearings in Revision Surgery.
5.3 Revision Outcomes after Ceramic Failure
5.4 Ceramic Heads with Sleeves for Revision Surgery
5.5 Revision Outcomes after Adverse Local Tissue Reaction to Metal Particles
5.6 Revision Outcomes using Ceramic Bearings
5.7 Revision Outcomes in the U.S. Medicare Population
5.8 Sumary
5.9 Acknowledgements
5.10 References
5.1 Introduction
Currently over 50,000 revision total hip procedures are performed annually in the United States, and the demand for revisions is projected to increase in the coming decade, especially among younger patients [1-3]. Ceramic bearings have a long clinical history in primary total hip replacement, and many published studies and international registries have documented successful long-term survivorship of these implants. However, less is known about the utilization and outcomes for patients treated with ceramic bearings during revision surgery.
In surveying the ceramic bearing literature, as described in Chapter 3.1, the vast majority of the 1750 papers we identified are related to primary surgery. Aside from case reports and review articles, relatively few studies have previously been published exploring outcomes of ceramic bearings in revision THA [4-13]. Previous studies focused on revision outcomes during special circumstances, such as revision after ceramic fracture [6, 11, 13]; revision in patients with osteolysis [7]; or revision after failed metal-on-metal hip arthroplasty [4]. As the demand for revision surgery is expected to increase, there has been interest in studying revision surgery outcomes for ceramic bearings in the general patient population [5, 8, 10, 12].
In this chapter we will review both the utilization and outcomes of ceramic bearings in revision total hip arthroplasty (R-THA). Because of the published literature on this topic is limited and heterogeneous, a somewhat different approach was taken in this chapter because a formal systematic review was not feasible to aggregate clinical results. This chapter dealing with revision surgery has been expanded to include a few references to recent and timely peer-reviewed conference abstracts, but only when necessary to address emerging topics that have not yet had sufficient time to reach the peer reviewed literature. We will clearly identify which studies are based on conference abstracts, and which have been published in refereed journal articles.
^ Return to Top
5.2 Utilization of Ceramic Bearings in Revision Surgery
We used the 100% Medicare inpatient sample administrative database to identify 31,809 Medicare patients who underwent R-THA between 2005 and 2013 with known bearing types. These data were presented in a conference abstract [12]. The relative usage of ceramic bearings in revision varied over this time period (Figure 5.1), coinciding with the decrease in popularity of MOM bearings due to reports of adverse local tissue reactions to metal debris. The usage of both C-PE and COC bearings in revision surgery increased substantially during this time period to 26.6% and 2.5%, respectively, in 2013 (Figure 5.1).
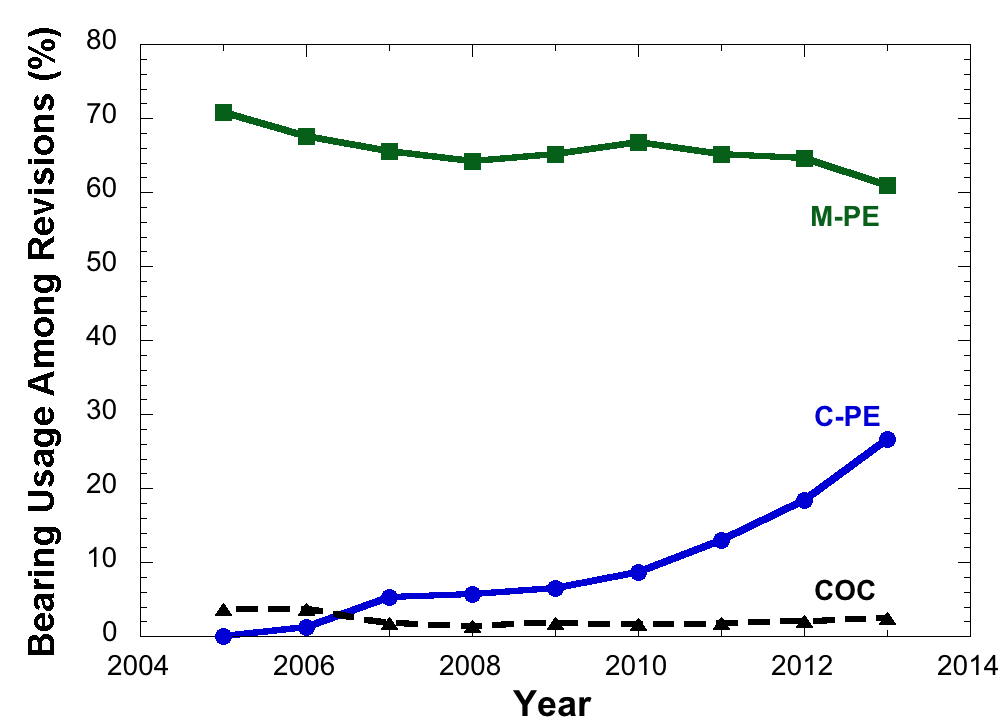
Figure 5.1.Reported bearing usage of C-PE, COC and M-PE in revision total hip arthroplasty in the U.S. Medicare population between 2005 and 2013 (% of all patients with revision codes)
The Medicare patients who received C-PE (40%, 65-69 years) and COC (31%, 65-69 years) bearings at revision surgery were generally younger than patients who received M-PE (23%, 65-69 years). There were fewer patients older than 80 years who received C-PE (18%) and COC (29%) as compared with M-PE (31%). Gender mix, however, did not vary much by bearing type. The Medicare patients who received C-PE (60%F) and COC (65%F) bearings were most frequently female, and had a similar gender mix as patients who received M-PE (60%F). These data indicate that ceramic bearings are being used in both genders and across the entire age range in the Medicare population, even in the oldest (80+ years) age group.
The utilization of alternative bearings has been previously examined in the context of primary THA and as result of concerns with MOM. Although the usage of MOM bearings has previously been studied in revision surgeries, we are aware of no previous utilization studies of ceramic bearings in revision for US patients, making comparison of the Medicare results difficult. Clinicians were attracted to alternative bearings due to the larger head sizes that could be achieved with MOM to improve joint stability and reduce dislocation risk. Since that time, larger diameter ceramic heads (up to 44 mm in diameter) are now clinically available in the US. Also, there is greater understanding based on international registry data that head sizes greater than 36 mm diameter may not necessarily provide improved dislocation risk in clinical practice. Finally, concerns with taper corrosion using CoCr femoral heads may also be playing a role in surgeon decisions to increasingly adopt ceramic heads in both a primary and revision scenario. While it is not possible for us to identify from claims data which of the abovementioned trends is responsible for the increase in ceramic bearing usage among Medicare beneficiaries undergoing revision, the trends are temporally coincident with the reduction of utilization of MOM bearings and, to a growing extent, reduced usage of M-PE bearings as well.
^ Return to Top
5.3 Revision Outcomes after Ceramic Fracture
The in vivo fracture of a ceramic component is a serious complication requiring immediate revision. The revision of a fractured femoral head may be complicated. A ceramic femoral head typically fractures into multiple fragments, which may be difficult for the revising surgeon to completely clean from the surrounding tissues. If not removed, residual ceramic particles can lead to third body wear of a subsequently implanted polyethylene liner or metal femoral head [11]. The morselised ceramic particles can also damage the trunnion of a well-fixed stem, necessitating its replacement along with the head and liner [6]. For these reasons, early attempts at ceramic fracture revision had variable and, in some cases, unsatisfactory outcomes [6, 11].
The earliest and largest series dealing with this issue was published by Allain and coworkers [11], who studied revisions performed after fracture from a ceramic femoral head by pooling data from 105 cases that occurred in 35 different surgical centers between 1977 and 1999. Published in 2003, their study included 18 cup designs from 14 manufacturers. The initial femoral heads were fabricated from alumina or zirconia, but the new heads were fabricated from stainless steel (the largest group), alumina, nitrated titanium alloy, reinforced stainless steel, cobalt-chromium, and zirconia. Overall, this is a very inhomogeneous group of cases spanning two decades of clinical history in France. The inhomogeneities in this group strongly limit the ability to apply these historical findings to contemporary implants in clinical use today. Notwithstanding these limitations, Allain and coworkers [11] concluded that: “The operative technique for the treatment of a ceramic head fracture was very variable in our series. Three parameters appeared to be important: cup revision, the material of the femoral head, and total synovectomy....” Therefore, Allain’s work supported the concept of third-body wear as a risk following ceramic head fracture, but the ability to make predictions about future implant survival appeared to depend upon both surgical treatment factors (e.g., complete synovectomy) and implant variables (e.g., the choice of femoral head material). Stainless steel femoral heads had the worst outcome after revision, as they could be eroded by third body wear. Allain and colleagues advocated the use of a CoCr or ceramic femoral head in revision surgery to address the risk of re-revision due to 3rd-body wear and recommended that the stem be saved unless the taper was severely damaged.
In 2010, Sharma et al. [13] described the long-term outcomes of revision surgery following ceramic head fractures. The primary surgeries in this small series of 8 cases were performed between 1990 and 1992 and 2nd-generation alumina, BIOLOX®, was used as the femoral head material in the primaries. Following fracture, the patients were treated emergently with a complete synovectomy. The patients all received a CoCr femoral head and a conventional polyethylene acetabular component at revision. The patients were followed after revision for 10 years, on average (range: 84-180 months). Two patients were lost to follow-up, one patient was revised at 12 months due to infection, and another patient was revised at 8.5 years due to periprosthetic fracture. Long-term radiographs were analyzed in five patients. The wear rate was 0.11 mm/y and was comparable to a matched group of 6 patients with a primary THA (0.14 mm/y, on average). The authors described their technique of achieving a complete anterior and posterior synovectomy, which they credited for the longevity of the revision surgeries with no evidence of 3rd body wear.
Traina et al. [14] described 40 COC patients who were revised due to fractured ceramic component between 1990 and 2009. As an AAOS Scientific Exhibit featured in JBJS, this paper highlights several of the fractures as case studies and offers treatment techniques for ceramic head and liner fractures.
In 2014, Koo and colleagues [6] reported the outcomes of patients who were revised after fracture of 3rd generation alumina heads (BIOLOX®forte). The authors contended that these modern ceramics were “much sharper and harder than early generation ceramics,” and that the early revision treatment paradigms may not be applicable to revising fractures with contemporary ceramic implants. They studied 24 patients who were revised for ceramic fracture between 2002 and 2009. In all cases, the Morse taper of the stem was visibly damaged with multiple scratches but was not removed in 20 cases, due to concerns about damage to the proximal femur. The 20 stem retained revisions were replaced with COC bearings in 4 cases and M-PE in 16. Among the 4 cases in which the stems were replaced, 3 received COC bearings and 1 received M-PE. There were no revisions among the four cases in which the stem was replaced. However there were five revisions in the stem-retained group: two subsequent ceramic head fractures, two cases of metallosis among the patients with CoCr heads, and femoral osteolysis and stem loosening in a fifth patient. The authors warned that neither ceramic or CoCr femoral heads should be implanted on a scratched stem taper due to the risk of subsequent revisions for fracture (in the case of a ceramic head) or adverse local tissue reaction (in the case of a CoCr head).
^ Return to Top
5.4 Ceramic Heads with Sleeves for Revision Surgery
It must be emphasized that the studies of revision surgery for ceramic fracture, described in the previous section, did not include the use of metal taper adapter sleeves, which were developed in the 2000s specifically to address the issue of encountering a stem taper that was damaged with a well-fixed stem. Due to the potential for trunnion damage, surgeons were once cautioned not to implant a new primary ceramic head during a revision if the stem is not also going to be revised.
In France there was some controversy regarding whether or not a trunnion should be re-used for the subset of revisions in which no visible evidence of taper damage can be detected at the time of surgery. Hannouche and colleagues [9] published a study in which they argued that “it is possible” for no ceramic fractures to occur on a well-fixed titanium trunnion, provided the surgeon performs a “careful inspection” of the trunnion for “major imperfections.” Their data were based on 110 routine acetabular revision cases, which included 7 ceramic liner fractures and only 1 ceramic head fracture as reason for revision. For ceramic heads implanted on well-fixed stems, no head fracture leading to re-revision was reported at an average follow-up of 88 months.. Hannouche and colleagues [9] provide no objective guidance or quantitative metrics for what they constitute a “major imperfection” of the trunnion. The only alternative to re-using the trunnion that Hannouche considered in their paper was complete revision of the well-fixed stem.
Today, metallic sleeves are now available to “regenerate” the taper in a revision surgery so that a new ceramic femoral head can be used. This option avoids the undesirable alternative of revising a well-fixed stem or re-implanting a ceramic head on a used trunnion, which is not recommended by device manufacturers. In vitro testing strongly supports the use of these taper adapters sleeves in the case of a fractured ceramic head [15], because the microscopic damage to the trunnion can be invisible to the naked eye, yet still negatively impact the fracture resistance of the revised head. An example of a “revision” ceramic head with a metallic sleeve is illustrated in Figure 5.2.

Figure 5.2.Comparison of a ceramic revision femoral head fabricated from zirconia-toughened alumina (ZTA) with primary ceramic heads (BIOLOX®option). The revision head has a metal sleeve to "regenerate" the trunnion of a femoral stem, which may have become damaged in vivo.
Because the risk of ceramic fracture has decreased with the introduction of alumina matrix composites (see Chapter 2), we are not aware of any modern studies examining the outcomes of a large series of fractured delta heads with sleeves. Instead, recent studies of revision surgery, including the use of taper adapter sleeves, have focused on the use of ceramic heads in routine all cause revision surgery [8, 16]. For example, Jack and colleagues [8] have published the outcomes of revision surgery using ceramic heads with taper adapter sleeves, but these revisions replaced polyethylene bearings due to osteolysis and loosening. In all cases, the femoral component was well-fixed, and the bearing was exchanged to COC. There were 100 alumina and 65 alumina matrix composite implants. With a mean follow-up of 4.8 years, the survivorship with any cause of failure was 96.6% for the acetabular component and 94.0% for the femoral component. The authors recommended the taper adapter sleeves as a useful tool for revision surgery.
^ Return to Top
5.5 Revision Outcomes after Adverse Local Tissue Reactions to Metal Particles
In recent years, there has been growing interest in the management of patients who are revised after adverse local tissue reactions to metal particles, either due to MOM hip bearings, or taper corrosion in M-PE bearings [4, 17, 18]. If a patient is revised secondary to an adverse reaction to metal, such as taper corrosion, there is a growing consensus in the clinical community that ceramic components should be used for the revision [17-19]. Initially the clinical evidence in support of this recommendation was indirect. For example, we know that taper corrosion and metal release will be mitigated by the use of ceramic head [20], as discussed in Chapter 4.5. However, there are only a few outcome studies that address revision outcomes after ALTR using ceramic bearings [4, 17, 18].
Researchers working in collaboration with the Australian registry examined the outcomes of revision of 844 MOM hip resurfacing procedures between 1999 and 2012 [4]. The most frequently reported reasons for the index revision were loosening, osteolysis, metal related pathology and fracture. There were 102 cases of re-revision in this cohort, and the overall risk of re-revision was 26% at 10 years. They found no difference in the risk of rerevision based on the bearing surface used in the index revision surgery. The most commonly used bearing surface in these revisions, ceramic on ceramic, had a re-revision rate of 14%. The hazard ratio for COC re-revision versus MOM was 0.46 (95% CI: 0.16-1.29), p = 0.141, which suggests a trend, but as reported was not statistically significant. Indeed, their study was underpowered to detect differences relative to a re-revision rate of 67% in cases where a MOM bearing was used in the revision surgery. The authors stated that an even larger number of patients than they studied would be needed to detect a difference in outcomes by bearing surfaces.
Researchers from Rush University in Chicago have described the treatment of a small series of patients who were revised with a M-PE bearing due to adverse reactions associated with taper corrosion [17, 18]. Their original case series included 10 patients [17], but recently, the outcomes for 27 revision patients with short-term follow-up have been published [18]. In 23/37 patients treated with a ceramic head and a Ti taper adapter sleeve, there were no recurrences of adverse local tissue reactions, whereas in the 4 patients treated with CoCr heads, there was one reoccurrence. Among 18 patients with two-years followup, there was a significant decrease in blood serum Co and Cr levels as compared with before revision. The authors advocated retention of a well-fixed stem and the use of a ceramic femoral head with a taper adapter sleeve as a reasonable option for the revision of M-PE hips secondary to adverse local tissue reactions and taper corrosion.
^ Return to Top
5.6 Revision Outcomes using Ceramic Bearings
We have seen that many of the previous papers dealing with revision outcomes for ceramic bearings have focused on specific but relatively rare indications, such as revision of a ceramic head fracture or revision of an adverse local tissue reaction. With the growth of revisions around the world and concern about the durability of revision surgery, there is a small but growing body of literature that focuses on the use of ceramic bearings for routine, all-cause revision surgery. These studies, which are summarized in Table 5.1, support that revision with COC bearings is not only safe and effective, but also highly successful, which some clinical series reporting over 95% survivorship without re-revision after 5-7 years follow-up. It is also clear from these studies that the risk of ceramic fracture following revision surgery is extremely low, even considering that most of the studies have documented outcomes for alumina COC bearings. Thus, the risk of fracture following revision surgery with COC appears to be acceptably low, comparable to primary surgery.
In general, the revision outcome studies are limited to single center series (Table 5.1), with the exception of the research by Khatod et al. [5], who followed the outcomes of revision surgery in the Kaiser Permanente integrated health system between 2001 and 2010. During this time period, there were 629 revision surgeries for a variety of reasons, of which 63 were re-revised (10%). Ceramic-on-highly crosslinked polyethylene (C-HXLPE) was used in the treatment of 13.7% (86/629) of the index revisions; metal-on-crosslinked polyethylene (M-HXLPE) was the largest treatment group (42.3%, 266/629). In examining the reasons for re-revision using multivariate Cox regression, they observed significant patient, surgeon, and implant factors. Among the implant factors, the use of ceramic head against HXLPE was found to significantly reduce the risk of re-revision (odds ratio: 0.32; 95% CI: 0.11 to 0.95; p = 0.04).
Table 5.1.Summary of clinical outcomes reported for ceramic bearings in revision THA.
| Study | Number of Hips | Index Revisions due to Aseptic Loosening (%) | Mean follow-up in years (range) | Bearing Used for Revision | Fractures | Kaplan Meier Survival (Re-Revision) |
| Hannouche et al. [9] | 110 | 83% | 9.3 (5 to 27) | COC, 28% (31/110); C-PE, 58% (64/110); M-PE, 14% (15/110) | - | 83.1% "revision for mechanical failure" at 10 years |
| Chang et al. [10] | 42 | 64% (27/42) | 5.4 (3.2 to 8) | COC, 100% (alumina) | - | 100% (no re-revisions) |
| Yoo et al. [7] | 64 | 59% (38/64) | 9.8 (7.0 to 13.1) | COC, 100% (alumina) | - | 96.9% at 7 years |
| Jack et al. [8] | 165 | 98% | 4.8 (2.1 to 12.5) | COC, 100% (100 alumina, 65 delta) | 2 alumina heads | 96.6% femur, 94% acetabulum at 8.3 years |
| Khatod et al. [5] | 629 | 14.3% | 5 | C-PE (13.7%) | - | 86.8% at 5 years |
| Kim et al. [] | 187 | 26% | 15.6 (11 to 19) | COC, 100% (96 alumina, 91 delta) | - | 93% at 15 years |
^ Return to Top
5.7 Revision Outcomes in the U.S. Medicare Population
The limited number of studies examining ceramic bearing outcomes after revision provided motivation for our orthopaedic health outcomes research group to study this topic in greater detail. We used the 100% Medicare inpatient sample administrative database to analyze the outcomes of 31,809 Medicare patients who underwent R-THA between 2005 and 2013 with known bearing types. These data were also presented in a conference abstract [12]. We used Cox regression incorporating propensity score stratification to evaluate the impact of bearing surface selection on outcomes, after adjusting for patient-, hospital-, and surgeon-related factors. We used a propensity score approach to adjust for surgeon bias in the selection of bearing types, because usually ceramic bearings are usually favored in younger, more active patients. By incorporating propensity scores into our statistical analysis, we accounted for surgeon preferences in assigning bearings to patients in the Medicare population. This allows for one of the most rigorous comparisons between patient cohorts treated with ceramic bearings and those with M-PE bearings.
For R-THA patients treated with C-PE bearings, there was reduced risk of 90-day readmission (Hazard Ratio, HR: 0.90, 95% CI: 0.84-0.96, p=0.007). We also observed a trend for reduced risk of infection with C-PE (HR: 0.88, 95% CI: 0.74-1.04) that did not reach statistical significance (p = 0.14). For R-THA patients treated with COC, there was reduced risk of dislocation (Hazard Ratio, HR: 0.76, 95% CI: 0.58-0.99, p=0.04). There was no significant difference in risk of re-revision or mortality for either the C-PE or COC bearing cohorts when compared with M-PE.
In this study of revision total hip surgery in the elderly Medicare population [12], we asked how the use of ceramic bearings changed over time and whether the type of ceramic bearing influenced outcomes relative to M-PE. Between 2006 and 2013, we observed an increase in the reported usage of C-PE and COC bearings in revision surgeries for Medicare beneficiaries. We found no evidence to suggest that ceramic bearings were associated with worse outcomes than M-PE when used in revisions. Conversely, we found support for our hypotheses that ceramic bearings may improve certain outcomes after revision surgery, such as 90-day readmission, dislocation, and perhaps infection; however the results were bearing- and outcome-specific. The findings of this study support further research into the association between ceramic bearings in R-THA and lower risk of hospital readmission, dislocation, and, potentially, infection.
^ Return to Top
5.8 Summary
In summary, ceramic bearings are now regarded as an accepted and successful option during many indications of hip revision surgery. The literature and our recent Medicare analysis also indicate that hip revisions using a ceramic bearing have at least as good or in some cases better outcomes than revisions with traditional M-PE bearings. Ceramics are now also thought to be especially useful in the revision of adverse local tissue reactions secondary to the use of MOM bearings or due to taper corrosion.
Regardless of the revision indication, the use of titanium taper adapter sleeves is strongly recommended to regenerate the pristine taper surface of the stem for mating with a ceramic head. There will inevitably be rare situations, such as in cases of gross trunnion failure [21], when the taper has been irredeemably damaged and even a taper adapter sleeve would not be suitable. For most cases, however, an adapter sleeve should be used for revisions involving a ceramic bearing.
5.9 Acknowledgements
The author would like to thank Doruk Baykal, Exponent Inc., for many helpful discussions as well as technical and editorial feedback on this chapter.
^ Return to Top
5.10 References for Chapter 5
[1] Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624-30. [2] Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606-12. [3] Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-5. [4] Wong JM, Liu YL, Graves S, de Steiger R. What Is the Rerevision Rate After Revising a Hip Resurfacing Arthroplasty? Analysis From the AOANJRR. Clin Orthop Relat Res. 2015. [5] Khatod M, Cafri G, Inacio MC, Schepps AL, Paxton EW, Bini SA. Revision total hip arthoplasty: factors associated with re-revision surgery. J Bone Joint Surg Am. 2015;97:359-66. [6] Koo KH, Ha YC, Kim SY, Yoon KS, Min BW, Kim SR. Revision of ceramic head fracture after third generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2014;29:214-8. [7] Yoo JJ, Yoon PW, Lee YK, Koo KH, Yoon KS, Kim HJ. Revision total hip arthroplasty using an alumina-on-alumina bearing surface in patients with osteolysis. J Arthroplasty. 2013;28:132-8. [8] Jack CM, Molloy DO, Walter WL, Zicat BA, Walter WK. The use of ceramic-on-ceramic bearings in isolated revision of the acetabular component. Bone Joint J. 2013;95-B:333-8. [9] Hannouche D, Delambre J, Zadegan F, Sedel L, Nizard R. Is there a risk in placing a ceramic head on a previously implanted trunion? Clin Orthop Relat Res. 2010;468:3322-7. [10] Chang JD, Kamdar R, Yoo JH, Hur M, Lee SS. Third-generation ceramic-on-ceramic bearing surfaces in revision total hip arthroplasty. J Arthroplasty. 2009;24:1231-5. [11] Allain J, Roudot-Thoraval F, Delecrin J, Anract P, Migaud H, Goutallier D. Revision total hip arthroplasty performed after fracture of a ceramic femoral head. A multicenter survivorship study. J Bone Joint Surg Am. 2003;85-A:825-30. [12] Kurtz SM, Lau E, Baykal D, Springer B. Outcomes of ceramic bearings after revision total hip arthroplasty in the Medicare population. Trans ISTA. 2015. [13] Sharma V, Ranawat AS, Rasquinha VJ, Weiskopf J, Howard H, Ranawat CS. Revision total hip arthroplasty for ceramic head fracture: a long-term follow-up. J Arthroplasty. 2010;25:342-7. [14] Traina F, Tassinari E, De Fine M, Bordini B, Toni A. Revision of ceramic hip replacements for fracture of a ceramic component: AAOS exhibit selection. J Bone Joint Surg Am. 2011;93:e147. [15] Guhrs J, Krull A, Witt F, Morlock MM. The influence of stem taper re-use upon the failure load of ceramic heads. Med Eng Phys. 2015;37:545-52. [16] Thorey F, Sakdinakiattikoon M, Thiengwittayaporn S, Windhagen H. Early results of revision hip arthroplasty using a ceramic revision ball head. Semin Arthroplasty. 2011;22:284-9. [17] Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655-61. [18] Plummer DR, Berger RA, Paprosky WG, Sporer S, Jacobs JJ, Della Valle CJ. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty. 2015;In press. [19] Carli A, Politis A, Zukor D, Huk O, Antoniou J. Clinically significant corrosion at the head-neck taper interface in total hip arthroplasty: a systematic review and case series. Hip Int. 2015;25:7-14. [20] Kurtz SM, Kocagoz SB, Hanzlik JA, Underwood RJ, Gilbert JL, MacDonald DW, Lee GC, Mont MA, Kraay MJ, Klein GR, Parvizi J, Rimnac CM. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471:3270-82. [21] Banerjee S, Cherian JJ, Bono JV, Kurtz SM, Geesink R, Meneghini RM, Delanois RE, Mont MA. Gross trunnion failure after primary total hip arthroplasty. J Arthroplasty. 2015;30:641-8.




